Please note this article is for information and educational purposes only.
There is no substitute for first aid training from a qualified professional or advice from a suitably qualified medical professional. In an emergency you should first contact emergency services in your local area. Though rare, medical emergencies can happen in the dental practice from time to time.
Recognising the early signs of a medical emergency and knowing how to manage the situation before outside help arrives can go a long way to ensuring the patient has a successful outcome. We would recommend all members of the dental team undertake emergency first aid training from a recognised and qualified provider. Here are seven common medical emergencies, the associated warning signs, prevention methods and treatment best practice.
Syncope (Fainting)
What is syncope?
Syncope is the most common medical emergency that occurs in dental practices. It has been estimated that syncope makes up around 60% of all emergencies. It results from a lack of oxygen or glucose to the brain. This can cause the patient to lose consciousness.What brings it on?
Syncope can be brought on by pain, anxiety and even the effect of low blood pressure when a patient gets up too quickly from the chair.What are the signs of syncope?
The early signs of syncope are nausea, perspiration and a fast heart rate (over 100 beats per minute). Signs of a more serious emergency include a drop in blood pressure, slow heart rate (under 60 beats per minute) and pupil dilation.How can syncope be prevented?
Ensure the patient has eaten a meal prior to their appointment to ensure they are not hyperglycaemic (blood glucose levels are too high). Apprehensive patients should be placed in a supine position when local anaesthetic is given.

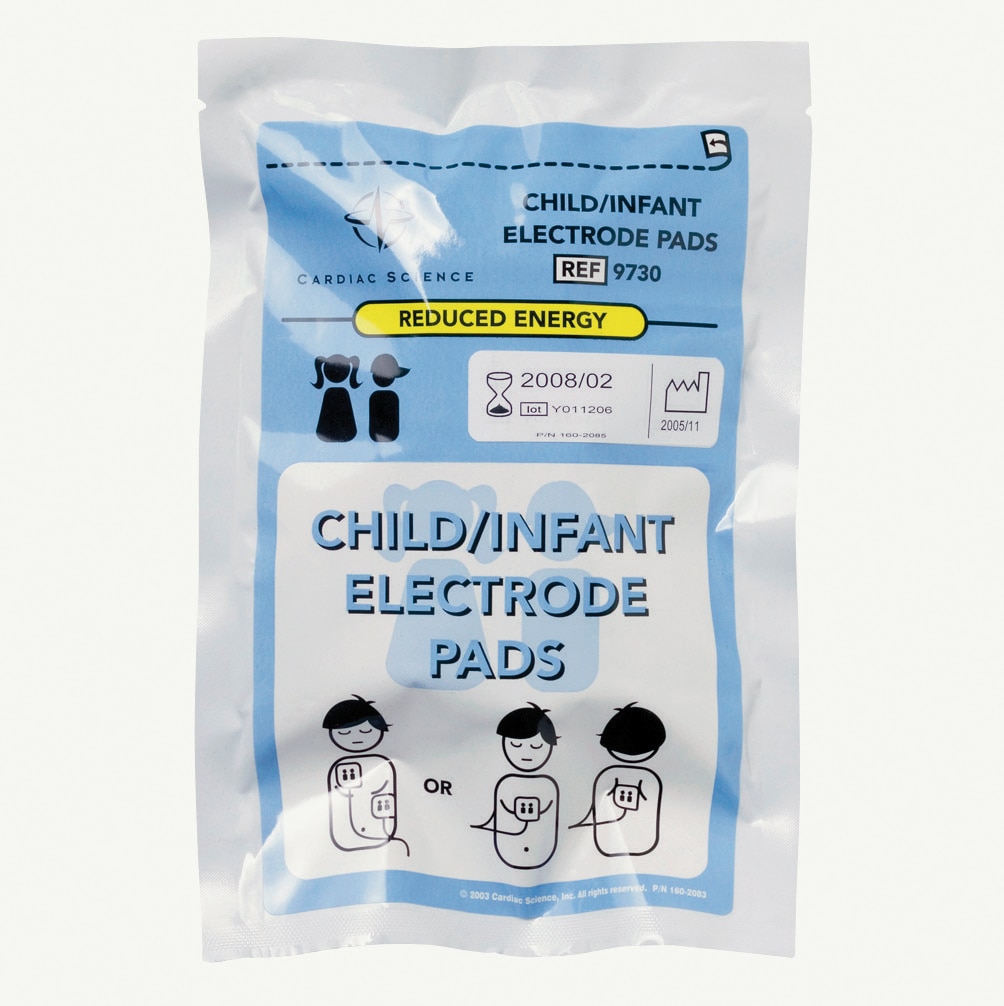
EcoLite Adult High Concentration Oxygen Masks With Tubing 24pk
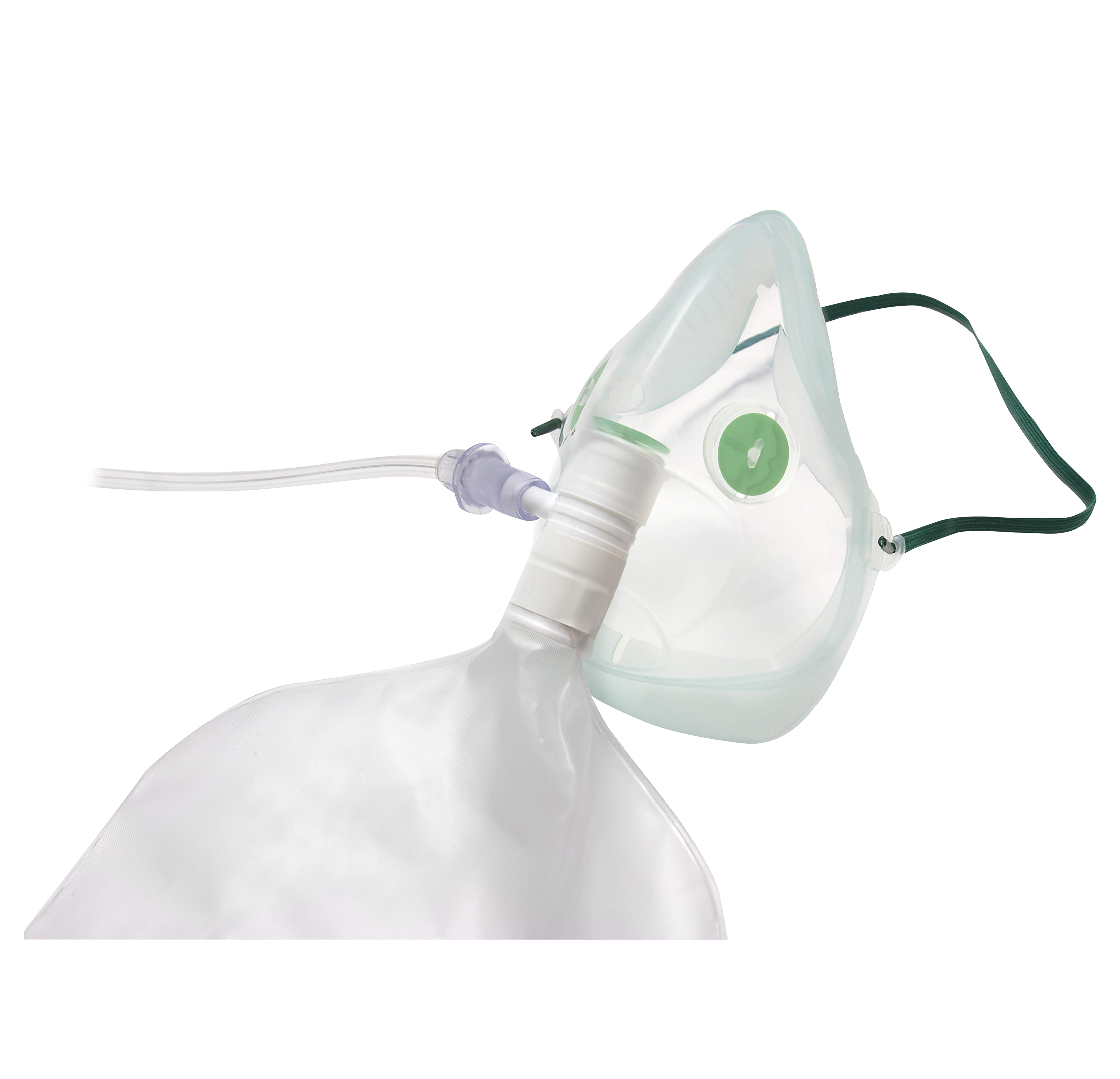
Intersurgical Adult High Concentration Oxygen Mask With Tubing Singles

Intersurgical Paediatric High Concentration Oxygen Mask with Tube
How Do You Manage a Syncope Emergency?
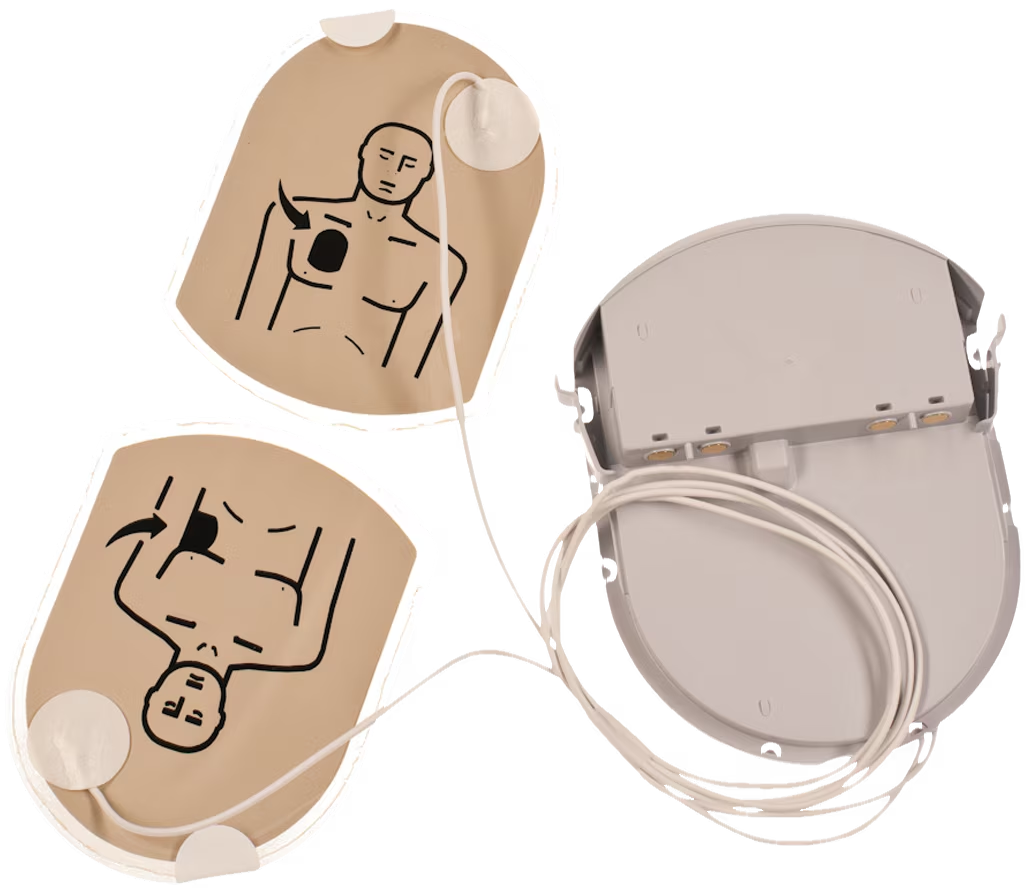
Syncope patients should be placed in a supine position and given oxygen. Airways should be maintained, and the patient’s blood pressure and pulse should be monitored until full recovery. If the recovery is delayed and the patient is conscious, a form of glucose can be given. If a patient does not respond, monitoring should continue, an ambulance should be called and CRP given by a trained member of staff.

EcoLite Adult High Concentration Oxygen Masks With Tubing 24pk
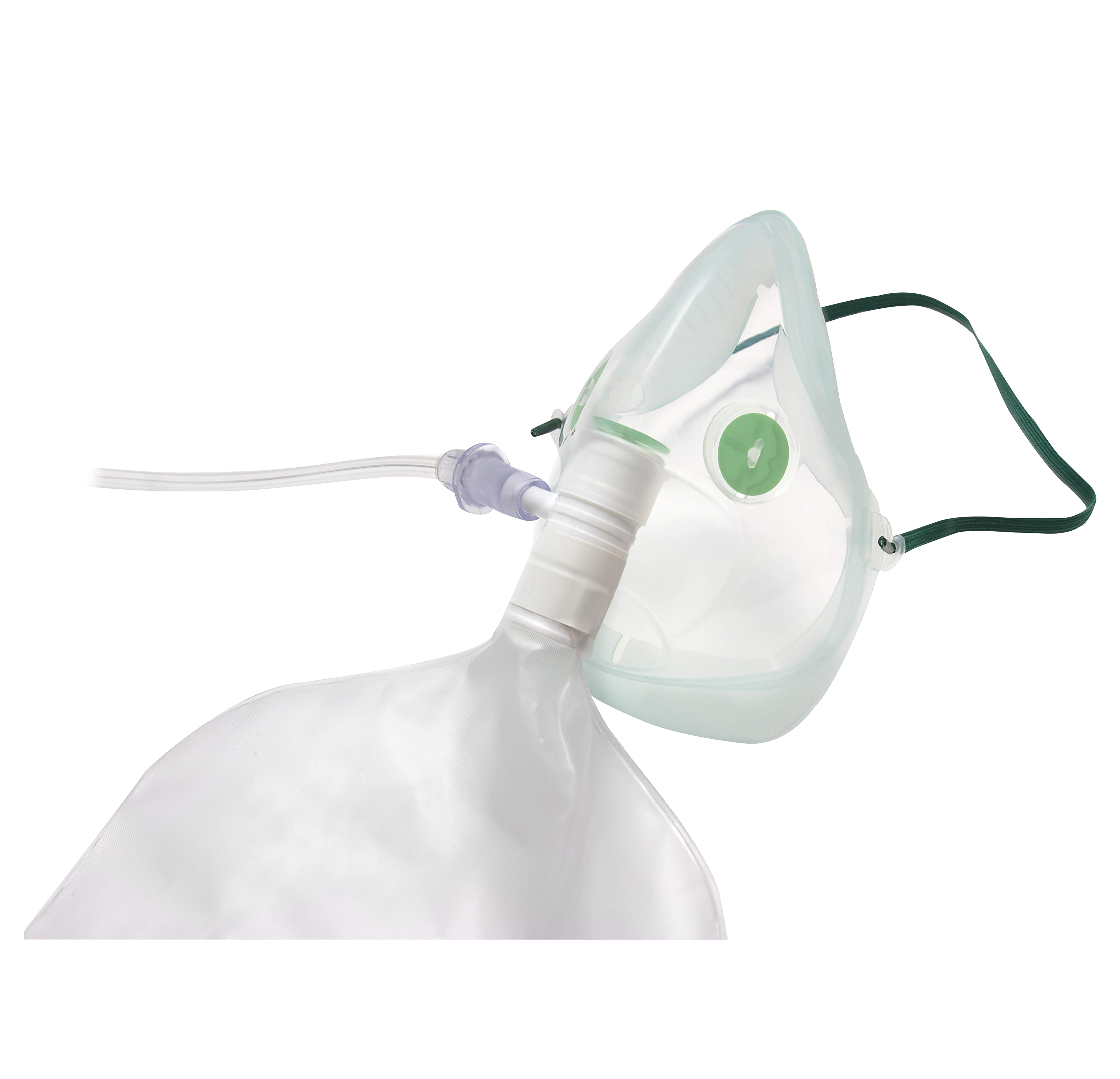
Intersurgical Adult High Concentration Oxygen Mask With Tubing Singles

Intersurgical Paediatric High Concentration Oxygen Mask with Tube
Hyperventilation (Panic Attack)
What is hyperventilation?
Hyperventilation is one of the more common medical emergencies. It is irregular breathing that occurs when a person breathes in more than the body needs.
What brings it on?
Hyperventilation is chiefly caused by anxiety. It will usually happen in patients who have a history of panic attacks which should be recorded in their medical record.
What are the signs of hyperventilation?
Rapid or deep breathing is the most obvious sign of hyperventilation. Another indicator that a patient may be prone to hyperventilation is if they are taking any anxiolytics (anti-anxiety drugs), such as diazepam.
How can It be prevented?
Remove anything that might be causing the patient stress, for example removing the needle out of the patient’s field of vision if you see them staring at it.
How do you manage a hyperventilation emergency?
Unlike other medical emergencies, hyperventilation patients should be placed in an upright position. Because the patient is blowing off carbon dioxide, you want to get this back into their system. This can be done by having the patient breathe into their hands, a bag or a mask with no flow of oxygen.

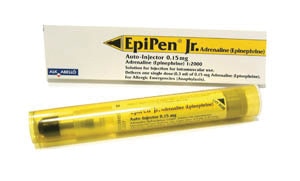
Allergic Reaction
What are allergies?
An allergy is where the body reacts to something that's normally harmless. Allergic reactions range from the minor type, for example dermatitis (skin irritation), to potentially life-threatening emergencies like anaphylaxis.What brings it on?
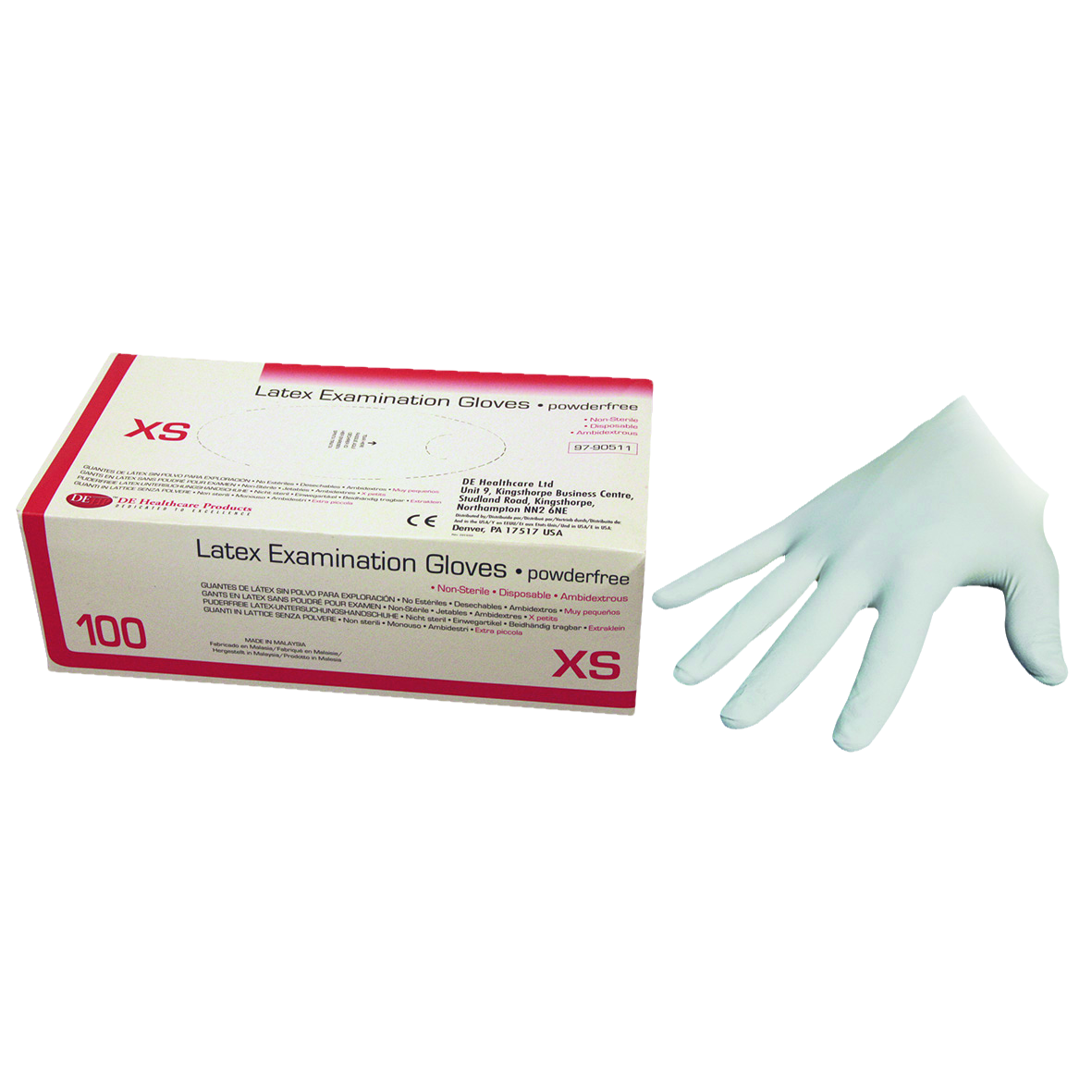
Allergic reactions happen when the immune system is challenged by an allergen. One of the most common allergies is latex, which can be found in some rubber dams and gloves.What are the signs of an allergic reaction?
Signs include itchy skin or a raised rash (hives), nausea, swelling (angioedema) and stomach pain. Signs of a more serious allergic reaction and potentially anaphylaxis include feeling faint, tongue swelling, breathing difficulties, wheezing, clammy skin, a fast heartbeat, low blood pressure and loss of consciousness.How can it be prevented?
The patient’s medical history is key to spotting the chances of an allergic reaction. See if they have any seasonal allergies, are allergy to any types of medication or if they have a history of asthma. Be prepared for patients with latex allergies by stocking latex free rubber dams, gloves and prophy brushes.Asthma
What is asthma?
Asthma is a common lung condition that causes occasional breathing difficulties. People with asthma have inflamed airways which are sensitive to things that may not bother other people. Asthma can sometimes get worse for a short time – this is known as an asthma attack.
What brings it on?
The most common asthma attack triggers include allergies, air pollution and other airborne irritants, and health conditions including respiratory infections. Strong emotions such as fear can also cause asthma attacks, along with certain medicines like aspirin and NSAIDs (nonsteroidal anti-inflammatory drugs).
What are the signs of an asthma attack?
Patients who suffer from asthma should have this noted down in their medical record. Lots of these patients will carry inhalers with them. Signs of an asthma attack include wheezing, breathlessness, a tight chest and coughing.
How can it be prevented?
Limit the chances of an asthma attack happening by making note of any allergies the patient has and then removing any potential irritant.
How to manage an asthma attack?
As soon as you spot signs the patient may be having an attack, suggest that they sit up and use their inhaler. Salbutamol Inhalers should be on hand in the practice to give to the patient in case they do not have one.
How to manage an asthma attack?
As soon as you spot signs the patient may be having an attack, suggest that they sit up and use their inhaler. Salbutamol Inhalers should be on hand in the practice to give to the patient in case they do not have one.

Salbutamol Inhaler CFC Free 100mcg 200 Dose

Salbutamol Ivax Inhaler 200 Metered Doses
Chest Pain (Angina)
What is chest pain?
Chest pain is one of the less common medical emergencies in the dental practice, but can be one of the most serious. Most chest pain is not a sign of anything serious, but it can also be a warning sign that the patient is at risk of a hearth attack or stroke.
What brings it on?
Stable angina is usually triggered by physical exertion or stress. It normally stops within a few minutes of resting. Unstable angina is more serious, may not have a trigger and can continue despite resting.What are the signs of chest pain?
Physical signs that the patient is experiencing chest pain include pressure, tightness or squeezing in the chest. If the patient’s pains start radiating down the left arm, both arms, to the neck, jaw, back or stomach, this could be signs of a heart attack. Other signs include a rapid heartbeat and difficulty breathing.How can it be prevented?
A patient’s medical history should have down if the patient has a history of chest pain. This should be viewed as a red flag that the patient may have an incident during treatment. If the patient is taking any diuretics, calcium channel blocks, beta blockers or any type of nitro-glycerine, this is another giveaway. Speak to the patient’s GP before treatment to talk through potential precautions and sedatives that the patient should have.
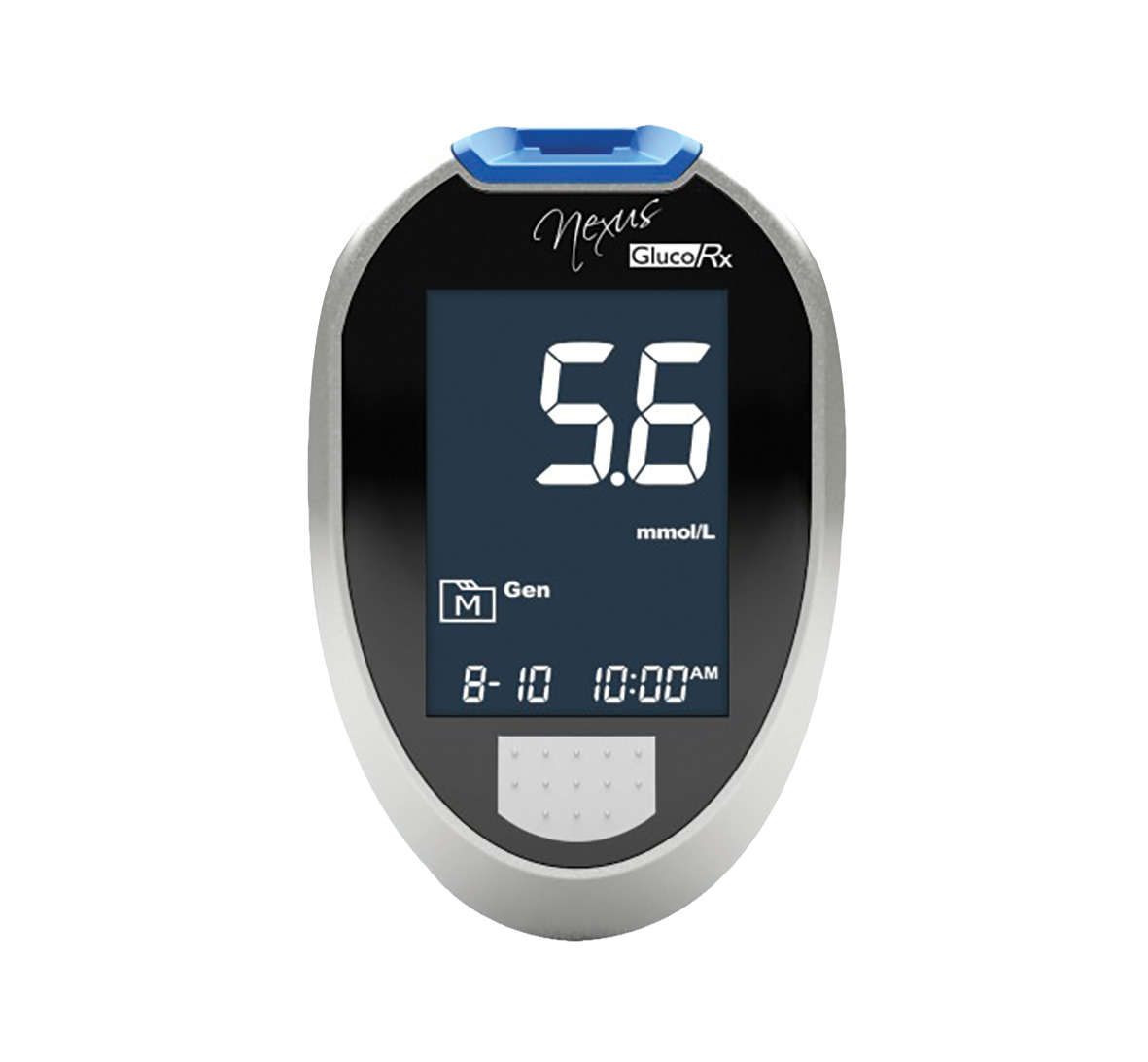
Hypoglaecemia (low blood sugar)
What is hypoglycaemia?
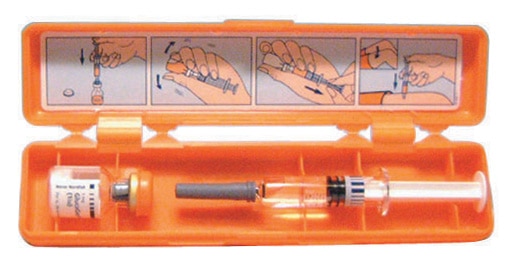
Hypoglycaemia is a type of diabetic emergency. It is where the level of glucose in the blood drops too low.What brings it on?
Hypoglycaemia can be cause by taking too much insulin, incorrect timing of taking insulin or by not eating enough carbs for how much insulin is taken.What are the signs of hypoglycaemia?
Early signs can include agitation, sweating, restlessness, shaking, a fast heartbeat and turning pale. If not treated, further signs can include weakness, blurred vision, seizures or fits and collapsing.How can it be prevented?
One way of preventing hypoglycaemia from happening is by making sure the patient has eaten recently. Some dentists prefer treating diabetic patients who do not have good control in the morning because they are more likely to have recently eaten and therefore have higher blood sugar levels.
Seizure
What is a seizure?
Seizures are one of the main symptoms of epilepsy. These are sudden bursts of electrical activity in the brain that temporarily affect how it works. There are several different types of seizures ranging from a simple partial seizure to a status epilepticus seizure which is a medical emergency that needs to be treated as soon as possible.
What brings it on?
Seizures tend to happen randomly to people who suffer from epilepsy, but they can also have certain triggers which include stress, alcohol, a lack of sleep and some medicines and drugs.What are the signs of seizure?
Symptoms depend on the type of seizure. General warning signs of a seizure can include staring, jerking movements, periods of rapid eye blinking, breathing problems and loss of consciousness.How can seizures be prevented?
Patients likely to suffer from a seizure will probably have a history of epilepsy recorded in their medical record. Patients who are hypoglycaemic are also potential seizure risks. Having this information on hand can help you to make the best decisions on treatment and manage possible risks. For example, some commonly prescribed antifungal agents and antibiotics can interact with anti-epileptic drugs which can jeopardize seizure control.
How do you manage a seizure emergency?
Start by removing whatever the patient had in their mouths and then move any objects or instruments away from the patient to prevent them causing injury to themselves or you. The seizure should then be allowed to take place and will usually last for a few seconds up to around a minute. Do not try and restrain the patient. If the seizure lasts for longer than 3 minutes that is when a benzodiazepine medication such as Midazolam can be given via an intramuscular or intravascular injection. The NHS advice is that those untrained to deal with seizures call an ambulance immediately if a patient has a seizure that doesn’t stop after five minutes.