What is a Dental X-ray?
A dental X-ray, or radiograph as it’s also known, is a procedure used to produce images of the inside or outside of a patient’s mouth. X-rays are used to provide a clearer picture of the health of the teeth, roots, gums and bones. Among other things, X-rays can detect tooth decay and bone loss, issues that a simple oral exam would unlikely pick up.
How Do Dental X-rays Work?
X-rays are a penetrating form of high-energy electromagnetic radiation. This energy can travel through or be absorbed by human tissue. After travelling through a dental X-ray machine tube and then human tissue, the photons (electromagnetic particles) reach a receptor at the other side. This receptor is traditionally a sheet of film which is processed in chemicals to then produce the X-ray images. Becoming more popular is the use of digital receptors which are able to process the images straight to a computer.
What Do Dental X-rays Show?
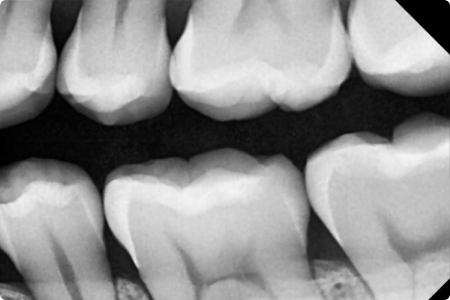
X-ray beams weaken as they travel through human tissue. The thicker the tissue, the fewer photons that make it through to the receptor. An X-ray image will show denser areas of the mouth, such as enamel and dentine, as light-coloured (radiopaque). Less dense areas, such as the pulp and gums, show up darker (radiolucent). Dental X-rays can spot the early signs of a cavity by the appearance of radiolucent (darker) patches in areas which should normally be white, such as the dentine.
Dark spots that appear between the roots of the teeth can show potential active bone loss or gum disease. Areas that are particularly white on an X-ray image are most typically fillings or crowns, as these are more radiopaque than even enamel.
Types of Dental X-rays
There are two main types of dental X-rays: intraoral X-rays and extraoral X-rays.
- Intraoral dental X-rays are taken with the receptor inside the mouth and are used predominately to examine the teeth and supporting structures.
- Extraoral dental X-rays are taken with the receptor outside the mouth and are used for looking at the jaw, skull and a panoramic picture of the patient’s teeth.
Bitewing X-rays
Bitewings are most effective at detecting cavities developing on and between teeth, and bone loss due to gum disease.
Periapical X-rays
Periapical X-rays are used primarily to diagnose abscess and cysts around the roots of the teeth, as well as disease in the surrounding bone structures.
Occlusal X-rays
Occlusal X-rays are used to detect tooth and bone fractures from trauma.
Panoramic X-rays
It can be used to study missing and developing teeth, jaw structure and wisdom teeth.
Cephalometric X-rays
It can be used to track growth and is particularly useful for orthodontic dentistry.
How Are X-rays Processed?

PSPIX2 Imaging Plate Scanner
How Are X-rays Processed?
A simple definition of CAD/CAM dentistry is the use of digital software to design and manufacture dental restorations and prostheses. CAD stands for computer-aided design and CAM stands for computer-aided manufacturing. The technology can be used to create crowns, dentures, inlays, onlays, bridges and veneers among other things. The speed of the CAD/CAM process allows for dental prosthetics to be designed, manufactured and delivered to the patient in quick time, sometimes the same day. The wider system of using computer assisted technologies to produce restorations is known as CEREC (Chairside Economical Restoration of Aesthetic Ceramics).

PSPIX2 Imaging Plate Scanner
Are Dental X-rays Safe?
Dental X-rays sit between ultraviolet radiation and gamma rays on the electromagnetic spectrum. The level of radiation given off by a dental X-ray and absorbed by a patient is minimal and lasts only a fraction of a second. Dental X-rays are therefore considered a very safe procedure. Advances in technology and the ability to target X-ray beams on smaller areas of the mouth have made the process safer.
It is important that the whole dental team is aware of radiation safety. The National Radiological Protection Board, Guidance notes for dental practitioners on the safe use of X-ray equipment (2001) should be used for guidance. A patient always has the choice of whether to proceed with a dental X-ray. Likewise, a dentist has a choice of whether to provide care to patients who refuse an X-ray. When this occurs, good documentation in the patient’s records is essential.
How Many Dental X-rays Are Too Many?
It is common for new patients to receive an X-ray during their first dental examination. The number of X-rays a patient requires thereafter will depend on individual medical and dental history. Some patients might require an X-ray every 6 months while others will only require one every couple of years. Examples of patients who might require more frequent X-rays include children, smokers, patients with gum disease and patients with lots of fillings.
Dental X-Ray UK Regulations
Dental staff in the UK are required by law to be IRMER trained. This applies to everyone involved in taking and/or processing radiographs. Practices are now also required to register with the HSE if they use radiographic equipment. The Ionising Radiation (Medical Exposure) Regulations 2017 (IRMER) relates to the protection of the patient and specifies that individuals are informed in advance of the risks of any ionising radiation exposures they receive.
There should be a clearly defined person at each dental practice responsible for implementing both IRMER and IRR99 legislation. This is often the practice manager. The Ionising Radiation Regulations of 1999 (IRR99), relates to the protection of workers, the public and the equipment aspects of patient protection.
From What Age Can Children Have a Dental X-ray?
There is no legal minimum age at which a child can have a dental X-ray. The decision on whether to give a child a dental X-ray is determined by the results of an oral exam and their dental history.
If a child’s teeth are close together and the dentist is unable to examine their health, a dental X-ray is typically recommended. Digital X-rays are suggested as a way of making sure a child patient’s exposure to radiation is kept minimal.
Can Dental Nurses Take X-rays?
Dental X-rays are normally taken by the dentist, but dental nurses can take an NEBDN course to become qualified to take X-rays themselves. More information can be found here.