What is Cross-Infection?
Cross-infection is the transmission of pathogenic bacteria, fungi, parasites or viruses (pathogens) from one place to another, either directly or indirectly.
Microorganisms can be transmitted in a variety of ways, including coughing and sneezing, touching surfaces, touching other people, through unsterilised equipment, unsanitary clothing or the prolonged use of intravenous lines.
Infection control procedures within a dental practice aim to prevent the transmission of infectious agents during patient care.
What is HTM-01-05
HTM 01-05 is the document from the Department of Health covering the standards of decontamination work required in dental practices. It was designed to raise the quality of decontamination procedures and ensure compliance across the industry.

Cross-Infection Control Measures
There are several important cross-infection control measures that all practices should implement. These include:
1. Hand hygiene
Hand washing with an appropriate hand sanitiser should be carried out before and after patient contact, procedures, donning PPE and before the cleaning of instruments or surfaces.
2. PPE
Patients should be provided with the appropriate Personal Protection Equipment (PPE) during their appointment. This is usually a bib, eye protection and a rubber dam when appropriate, and this may need to be changed should it become soiled.
Dental nurse PPE can include scrubs, gloves, eye protection, disposable aprons and face masks. PPE should not be worn outside of the practice and items that are not single use should be washed according to the manufacturer’s instructions at the highest possible temperature.
3. Ventilation
The dental surgery should be well ventilated to combat the infection risks posed from aerosol generating procedures (AGPs). High-volume suction should also be used when appropriate for aerosol control. Current fallow time guidelines should be adhered to in order to aid infection control.
4. Manual Cleaning
Dental instruments can be hand cleaned using an appropriate detergent prior to sterilisation. Warm water should be used at no higher than 45 degrees Centigrade.
5. Washer Disinfectors
Automated cleaning using a washer disinfector is widely considered the most effective solution for cleaning dental instruments prior to sterilisation. Using a washer disinfector enables a fully audited and validated process for regulatory compliance. Manufacturer’s instructions should be followed and an appropriate detergent used.
6. Ultrasonic Bath
Ultrasonic baths are widely used in dental practices prior to sterilisation. They use high frequency soundwaves to kill bacteria and other pathogens. Ultrasonic cleaners can be more effective than manual cleaning, especially on complex and hinged instruments. They can also reduce the chances of splashes and sharps injuries.
7. Sterilisation
Once cleaned, dental instruments should be sterilised using an autoclave. Autoclaves use steam and pressure to kill stubborn viruses. Sterilisation of Dental Clinical Guidance (SDCEP) guidance advises a temperature-pressure-time relationship for all small steam sterilisers of 134–137°C, 2.1–2.25 bar gauge pressure for at least a 3-minute holding time.
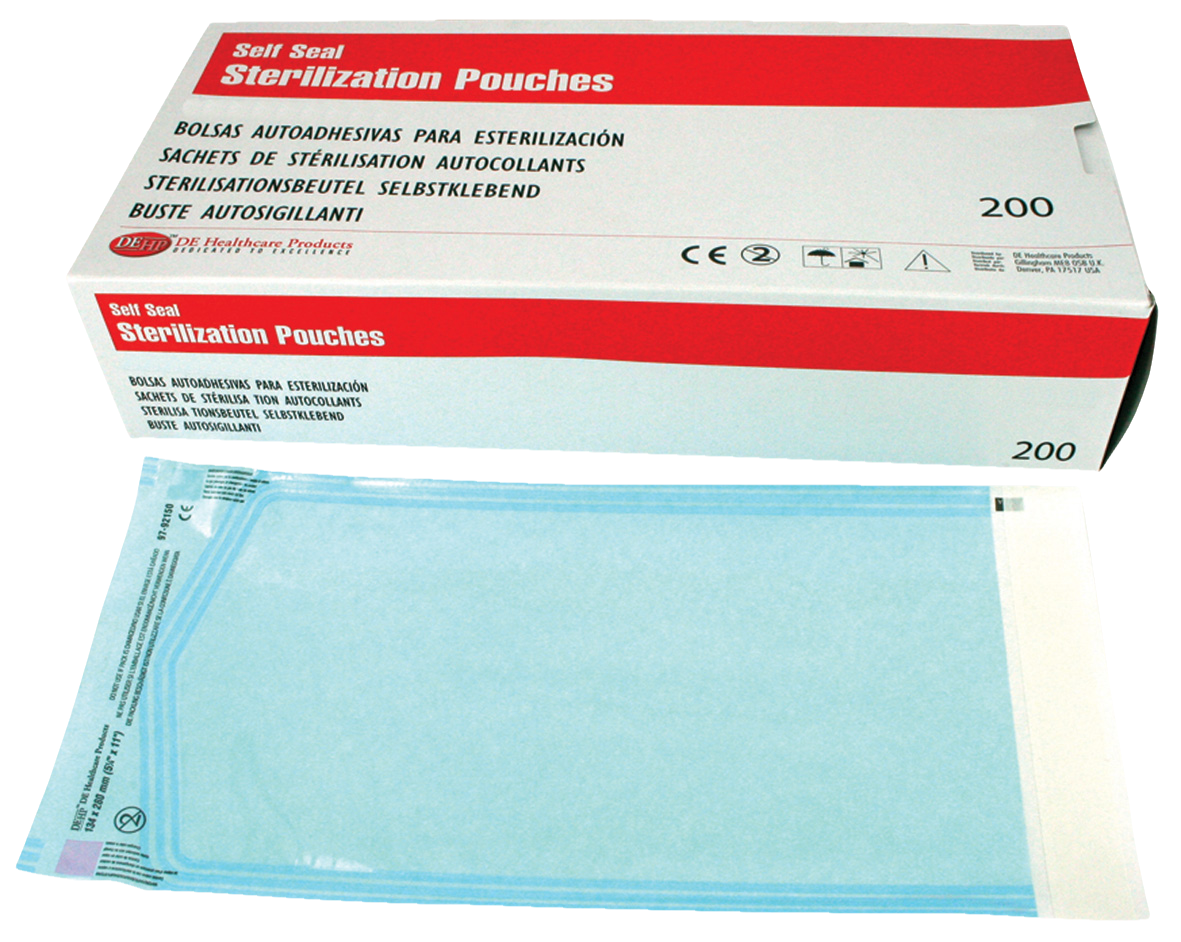
8. Packaging
Sterilised, dry dental instruments can be sealed in appropriate pouches and kept for 12 months before use. Unpouched instruments can be kept in a covered, airtight container in a non-clinical area for one week. Instruments should be packaged away from cleaning areas to reduce cross-infection risk.
9. Waste management
Clinical waste (blood or saliva contaminated waste) should be disposed of in orange clinical waste bags. Used sharp items should go in a Sharps Box and amalgam contaminated items in amalgam waste. A competent waste disposal company should be contracted to remove the waste from site.
It is the responsibility of the entire dental team, including dental nurses, to follow the latest Control of Substances Hazardous to Health guidance (COSHH) when handling or disposing of waste.
10. Zoning
Clear zoning areas for dirty to clean workflow are essential to ensure infection control compliance and reduce the risk of cross-infection between dirty and clean instruments. A designated dirty zone should be used for cleaning the instruments. This should be the location of the sink, washer disinfector and ultrasonic bath.
The autoclave is then next in the workflow, followed by a separate clean zone for pouching the clean instruments.
11. Schedules, Checklists & Audits
An infection prevention schedule should be in place and a checklist on hand to help ensure a safe working environment. Checklists should have separate sections for opening the surgery and closing the surgery and include tick boxes for all key infection control measures, i.e., PPE, sharps safety and sterilisation.
The Department of Health has a dental audit tool available to download for free to help your practice fight infection effectively. Download here.
12. Infection Control Lead
All practices should have a nominated infection control lead to ensure all staff follow the correct infection control protocols and receive appropriate training. It is worth getting the Basic Guide to Infection Prevention and Control in Dentistry book.
Disposable Cloths

DEHP Lint-Free Dry Cleaning Cloth 32 x 36cm 25pk
Disposable Cloths

DEHP Lint-Free Dry Cleaning Cloth 32 x 36cm 25pk
Disposable Wipes

Biocleanse Ultra Disinfectant Wipes Refill 200pk
Disposable Wipes

Biocleanse Ultra Disinfectant Wipes Refill 200pk
Hand Cleaners

Dentigel Alcohol Based Hand Disinfectant 500ml
Hand Cleaners

Dentigel Alcohol Based Hand Disinfectant 500ml
Sterilisation Pouches
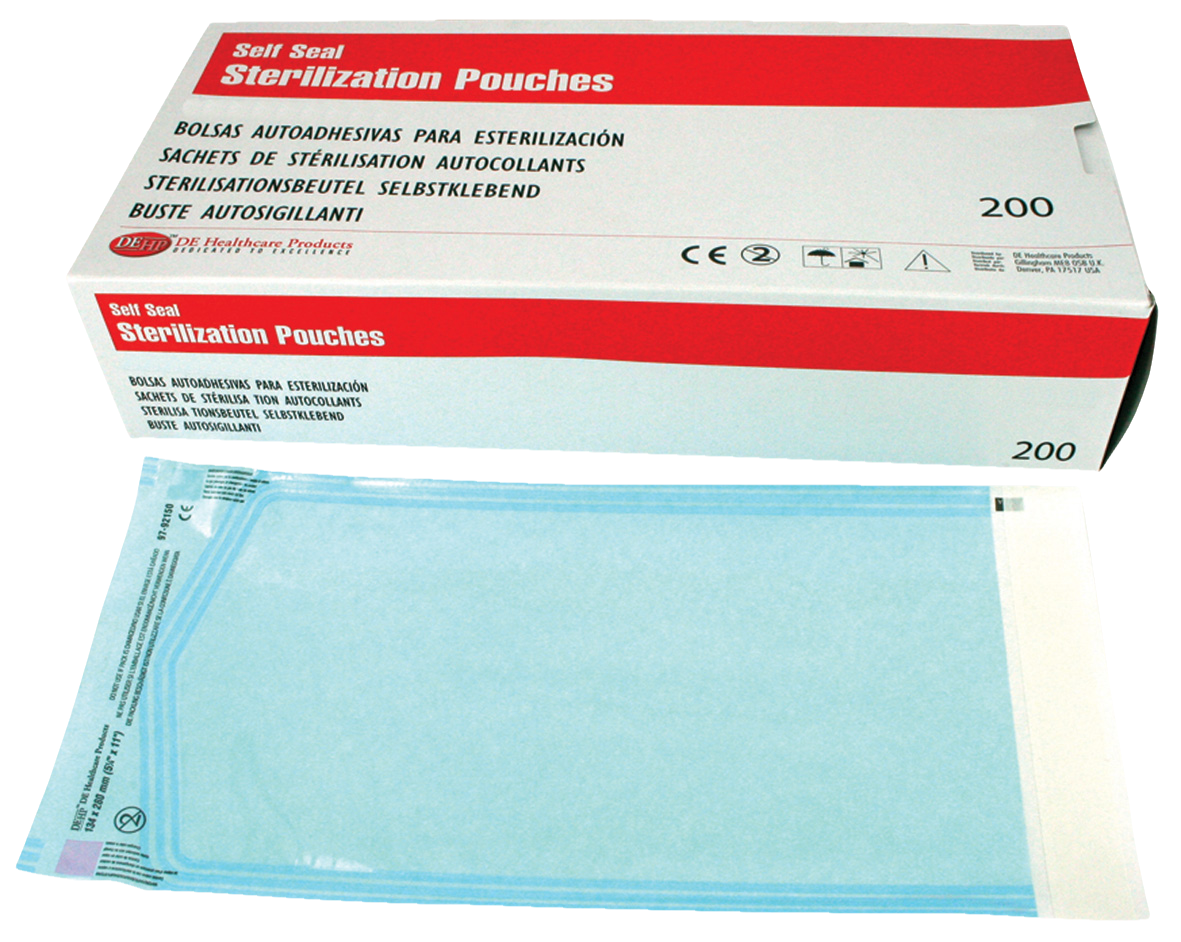
DEHP Sterilisation Selfseal Pouch 89 x 254mm 200pk
Sterilisation Pouches